Angel Fund Helps Puppy Stricken by Parvovirus

Victoria Romero, a young graphic design student, had wanted a dog since she was eight or nine years old. When she turned 16 a couple of years ago, she suggested to her mother that she give her a dog instead of a Sweet Sixteen party.
Her mother said no. “So I had never had another opportunity [to have her own dog] until now,” she said. A friend of her Mom, who had a female Maltese-Poddle mix puppy, wanted to find someone who could take the dog off her hands.
Victoria took charge of Kona in mid-November. The dog was lethargic and she knew that the animal would need shots. “So I called the [Aliso Animal] hospital and made an appointment for the next day,” she said.
Dr. David Bahou examined the dog and told Victoria that her new pet had parvovirus. “This is my first dog and I really wanted to be careful with her,” she said. “I was crying the whole time in the hospital because I thought maybe I had done something wrong.” At the time, she had been Kona’s owner only a couple of days.
Dr. Bahou assured her that she was not at fault. “He said that Kona’s symptoms would have started five to seven days after exposure so she had gotten the virus when she was with the previous owner,” Victoria said.
But there was another issue: paying for Kona’s treatment.
“I was very sad because I did not have the money I needed,” Victoria said, “and the only option was putting her down. I did not want to do that. I was already so attached to her. I loved her so much that I couldn’t do that. I called my family and friends to invite them to give me a little bit each.
“Dr. Bahou and the hospital staff really wanted to help me,” she said. “When they told me about Angel Fund, I said let’s do that. I just didn’t want to see Kona get worse because she already was so lethargic.
“I’m really grateful for Angel Fund and what they did. It really helped me out. I hope other people can find out about Angel Fund.”
Victoria, a student at Laguna College of Art and Design, works as a baby sitter for her mother and in a child day care role at a local school district. She expects to graduate from her program in the spring of 2025.
She heads to one of the schools in the district each work-day morning to help young students who participate in a pre-school program, she said. “I work about an hour and a half,” she said, “getting their minds awake for school.” Then she returns home to supervise her two younger siblings while her mother works.
Her mother does house cleaning and some gardening work and manages a group of workers.
Kona who is now about five months old and weighs about three pounds, is doing well. “She’s now about 100 percent,” Victoria said. “She has been running around the house trying to steal our shoes.”

Angel Fund Helps Mitzy, Blind Dog Diagnosed With IMHA

Helen Uitermark lives alone in her home in the San Gabriel Valley, except for her pets, including dogs large and small. About a year ago, she adopted Mitzy, “so, if nothing else, I can hug her on my lap.”
Mitzy is a West Highland White Terrier mix and is about the size of a Maltese-Poodle mix. She was just the right medicine to lift Helen out of a depression arising from her own medical problems.
Helen, is a senior citizen who often uses a cane or walker because of a broken ankle suffered nearly a year ago. Mitzy replaced two tuxedo cats that were apparently lost to coyotes.
Last spring, Helen said, “it was obvious that Mitzy wasn’t feeling well so I took her to Covina Animal Hospital. The diagnosis was glaucoma in her left eye.”
Dr. Karryssa Fenderson-Joseph, the hospital’s medical director, said that, when Mitzy’s condition did not improve with medical management, the best option she could offer was to remove the eye. The surgery took place a few days later.
Mitzy soon was able to run around in Helen’s backyard. “Everything was fine for several weeks,” she said. “Then, because Mitzy didn’t seem to be herself, I checked her, and the other eye seemed to have a white haze across it. I took her back to the hospital and she was diagnosed, again with glaucoma.” Dr. Fenderson said she recommended removal of Mitzy’s remaining eye after Helen told her that she didn’t want Mitzy to have on-going problems.
“After removal of the right eye, Dr. Fenderson had me come back several times because of an anemia condition (Immune-Mediated Hemolytic Anemia). I had never heard of it.
“Dr. Fenderson gave Mitzy a full-blood transfusion,” Helen said, “and she improved every week. We’ve been back to the hospital every month for a checkup. According to the doctor, the numbers have been holding so – unless something else happens – we’re good to go!”
Dr. Fenderson said that Mitzy has done so well since her transfusion that she is in remission and no longer is taking medication for IMHA.
Helen had been told about Angel Fund by friends and she asked Dr. Fenderson about it. “She immediately said: ‘Let me see what I can do.’ There was no further discussion about it but a few visits later, she said: ‘By the way, the grant has been approved.’ I almost danced out of her office! You have no idea how much I appreciate the Angel Fund grant.
“Dr. Fenderson has been so terrific, that’s where I will be going. It’s 15 miles from my home but, yes, she will be taking care of all my animals. I love her dearly.”
Mitzy seemed to be depressed after the second eye was removed. “She wasn’t interested in much and wasn’t even exploring. I was offered a kitten, about eight weeks old, and I said yes, since I’d lost the two cats last year.
“The kitten, Rusty, a male who is about six months old, and Mitzy get along fantastically. Mitzy’s depression has improved so much. It was wonderful to see. She gets around the house and backyard just fine. Every day her awareness seems to get better.”
Helen is getting used to dealing with a sightless Mitzy and she often forgets that her dog is blind. “She and I are getting accustomed to it. I can hear Mitzy on the other side of the door when I drive into the garage. It’s as if she’s trying to jump into my arms when I come through that door – then she does.”
But the household got a shock when Helen was pressured into accepting two Shi Tzu dogs that needed a new home. Helen said that she really did not want more pets, especially with a pinched sciatic nerve that added to her mobility problems. “They were absolutely loveable animals but it was too much,” she said.
A month after they arrived – the Shi Tzus were adopted by another family – much to Helen’s relief.
“My household is down to Mitzy and Rusty now. After the Shi Tzus left, Rusty came over to Mitzy when she was lying down and cuddled up to her. And she is walking through the house like it’s her domain again. I hope it is for many years to come!!”
Angel Fund Helps Shed Light On Vishnu’s Heart Problem

When Leticia Shaw’s cat, Vishnu, had a urinary blockage that required surgery about three years ago, the veterinarian told her that the condition sometimes can come back.
“Ever since then, I’ve been really anxious about that,” Leticia said. She has gotten regular checkups for Vishnu to make sure that doesn’t happen again.
During one of those checkups this spring at Little Tokyo Pet Clinic, Dr. Mary Chung told Leticia that Vishnu had a heart murmur. She recommended testing and x-rays to determine how severe the problem might be.
“That’s when Dr. Chung informed me about Angel Fund,” Leticia said. “I applied for a grant. The entire staff helped me with that process. Thankfully it was approved right away. I thought it would take way longer than it did.”
The tests showed that Vishnu has a cardiac problem. “They were able to do all the cardiovascular checks. But, basically, they just mentioned to me that he does have the problem – and once he has it, there’s no going back,” Leticia said.
“Thankfully, it doesn’t seem like it’s too serious. They caught it pretty early and they have given me heart medications and instructions on how to keep an eye on him to make sure it doesn’t get worse.
“There are warning signs like he might stop eating or when he sleeps his heart might beat too fast. So they gave me a couple of things to check. But honestly, he’s been amazing. He’s been super normal – he plays, he’s still himself. So hopefully it’s something that won’t get serious and we can just keep it contained.”
Leticia is grateful that she knows about the issue. And, she said, “thank God, things are going pretty good. I’m not seeing any signs for concern.”
She also expressed her gratitude for the Angel Fund grant and what it did to give her peace of mind and to help pay the veterinary bill.
Vishnu is seven years old and Leticia is optimistic that he has many years ahead of him. “He’s just so carefree and I hope he lives to 20. I can’t see him having any other problems. He’s now on a veterinary-prescribed diet and he can’t eat anything else.” But, she said, “the really scary problem for me was the urinary blockage.”
Leticia works as an IT manager for the Downtown LA Proper Hotel.otel.H Besides Vishnu, she has three dogs. She and her animals live in North Hollywood.
Angel Fund Grant Helps ‘Lucky Dog’ Get Surgery

Cheri Hanshaw, a fourth-grade teacher in Lancaster, owns a Shar Pei mix that she calls her lucky dog. “Star is my lucky dog because she gets everything to happen to her,” she said.
The last couple of years, she said, Star has had veterinary bills of about $10,000, include more than $3,000 a year ago when she was hospitalized with pancreatitis. The dog also has allergy problems. “We’ve had one thing after another with her,” Cheri said. “She’s usually at the vet’s every month.”
The latest iteration of her dog’s all too familiar relationship with veterinary medicine was recent surgery for a TPLO plate reaction, something that doesn’t happen often. Cheri did some research, which showed that it only occurs to about one in 50 dogs.
“Basically she had an infection from the plate in her knee and ite had to be removed,” Cheri said. “This is her second knee [to undergo TPLO surgery]. The left knee was fine and there was no problem after it was done a couple of years ago. And we had surgery in November for the right knee. It seemed fine and then after a few months, all of a sudden her leg started swelling up.”
Star, who is eight years old, is a patient of North Valley Veterinary Clinic in Lancaster. Dr. Eric Wright, who had done the TPLO surgery, told Cheri that the site infection could be treated with antibiotics but that it would continue to come back. “He recommended taking the plate out surgically so we don’t have to continue with these problems and spend all this money and then have to take it out surgically anyway,” she said.
Dr. John Chang, who assisted with the plate removal, told Cheri that he could see where an infection pocket was attached to a bolt on the plate.
The latest surgery took place in March. Because of Star’s history of medical problems, Cheri sought help from Angel Fund to help pay for the surgery. Dr. Misty Hirschbein, who sees Star for most of her appointments, told Cheri about Angel Fund and helped her apply. A grant of $1,000 was approved.
Cheri expressed gratitude to both Angel Fund and the North Valley Clinic, which matched the grant. But she also had to take out a loan to pay what she still owed. “I’m so in debt for this dog!” she said.
Star was still healing a month after the procedure, she said. “We had expected it would be healed by now,” Cheri said. “But the infection is almost gone.
“Star, the poor thing, has been living in a playpen since October. She has not been able to go outside to be a dog. She waits for us to come get her. So when I’m doing my school work, I’ll pull her out so she’s closer to me and not so isolated. I’m hoping she’ll be able to go back outside in a couple of weeks.”
Cheri lives with her daughter Kayla, who is a community college student. Her son, Zachary, She has a lives independently.
She previously had borrowed from her mother and taken out a loan from her credit union to help pay for her dog’s care. But Cheri is hoping things will change.
“I’m looking forward to being able to take Star on hikes again and to do the things that we used to do, like going to the beach. She’s almost there.”
If you would like to donate to the Animal Health Foundation to help more dogs like Star CLICK HERE or scan this QR Code

Angel Fund Helps Apollo Get Monthly Treatments


Ludovic Pathoux, who came to the United States from France in 2002, adopted Apollo, a beautiful white Pit Terrier, that he saw being neglected by a neighbor near his Los Angeles apartment some nine years ago.
“In 2014, while I was walking my American Bulldog Georgia, I saw Apollo behind the fence of one of my neighbors,” Ludovic said. “He was lying in the sun for hours at a time and was left out both day and night. I spoke to the neighbor about Apollo and his risk of getting skin cancer because of his exposure.”
The neighbor told Ludovic that she would like someone else to own the dog. “Despite already having a dog and difficult finances, I decided to adopt Apollo,” Ludovic said. “I simply fell in love with him and wanted to rescue him from his neglectful owner, even though I should not have had two dogs in my situation.”
Ludovic and the two dogs moved to an affordable cabin in the San Bernadino Mountains not long after Apollo joined the family. A couple of years later, Ludovic moved to an apartment in Yucaipa with Georgia and Apollo. A year later, he said, “my beloved Georgia died of cancer.”
Six months later, Apollo had a mole-like cancer on his leg that was removed by a veterinarian. And a few months later, Apollo was diagnosed with a tumor on his spleen and a splenectomy was performed to remove it. Georgia had a similar surgery a few years earlier.
In 2022, Apollo was diagnosed with chylothorax, a condition in which lymph fluids leak from his thoracic duct into the space around his lungs. Dr. George Makar at Yucaipa Animal Hospital made the diagnosis. Apollo is being treated there about once a month through thoracocentesis, a process in which a tube is inserted into his chest cavity after sedation to remove the fluids. The treatments started a year ago at a cost approaching $750 a month.
“Fortunately the procedure does not worsen his health nor does it cause pain or suffering,” Ludovic said. But the cost of his dog’s treatment is worrisome. Ludovic has had difficulty finding work as an organizer, who can make sense of your garage, pantry or spare room. (His website is http://www.ludovicorganizing.com.)
“I am not working every day so it’s up and down,” he said, and his erratic income prevents him from doing a lot of things he’d like to do, though he gives his dog’s health priority.
With Apollo’s crucial treatments in danger, Ludovic found Angel Fund with help from the Yucaipa hospital. He applied for a grant and Angel Fund provided $1,000 for Apollo, which was matched by the hospital.
“I sincerely thank the Angel Fund and Dr. Makar for generously helping me with this financial assistance,” Ludovic said. “Apollo greatly enjoys human beings and despite the invasive monthly treatments, he loves to go to the vet and is very excited to be around the assistants and technicians who give him lots of attention.
“My unconditional love for him has motivated me to do everything I can to increase his life expectancy.”
One of the reasons Ludovic does not want to return to France is that he would not be permitted to bring Apollo with him, nor could he have taken Georgia. He is intensely loyal to his animals.
But he said: “I choose to stay in the United States because I am all right here.” And he said, some 22 years ago “when I lived in Paris, I wasn’t happy.”
Boydston Senior Grant Helps Lulu Find New Lease on Her Life

Noreen Sturges, who lost her 15-year-old canine companion Papillon last year, found a replacement a few months ago in Lulu, a female Maltese. “Lulu was rather matted, had a hacking cough and needed care and lots of love,” Noreen said.
Lulu had belonged to a family that was no longer able to provide her with the care and attention she needed. When Lulu was brought to Noreen’s home, “it was love at first sight,” she said.
Noreen hired a groomer to attend to Lulu’s matted hair. After the grooming, Noreen took Lulu to Monarch Veterinary Hospital in Laguna Niguel not far from her home.
Dr. Kelly Alcala examined her and found some serious dental issues that would require surgery and the extraction of some teeth. Lulu also had a hacking cough – “not like she would have had with a cold,” Noreen said. Dr. Alcala told her that she thought decay from the dog’s teeth was getting into her digestive system and probably causing the cough, Noreen said.
The doctor suggested that Noreen apply for a Boydston Grant to help pay for Lulu’s treatment and surgery. A grant of $500 was approved and Dr. Alacala did the surgery. The dog is now thriving, Noreen said, and the hacking cough is gone.
Lulu is eating her new diet voraciously. “And she’s a love!” Noreen said. “Everything’s good now.” The dog, she said, “is running around – up and down the stairs and all over the place.
“I didn’t think I could ever love a dog as much as my Papillon, “but I just love Lulu.”
She added that she is grateful for the help provided by her Boydston grant and the matching sum from Monarch Hospital, as well as for the work of Dr. Alcala. “I just love her, too,” she said.
Noreen said that she and Lulu “are having a lovely time together. She is quite a companion.”
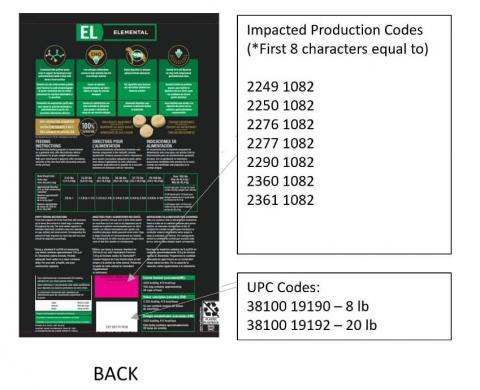
PURINA PRO PLAN RECALL

Nestlé Purina Petcare Company Voluntarily Recalls Purina Pro Plan Veterinary Diets El Elemental Dry Dog Food in the U.S. Due to Potentially Elevated Vitamin D
Nestlé Purina PetCare Company is voluntarily recalling select lots of Purina Pro Plan Veterinary Diets EL Elemental (PPVD EL) prescription dry dog food due to potentially elevated levels of vitamin D. Vitamin D is an essential nutrient for dogs; however, ingestion of elevated levels can lead to health issues depending on the level of vitamin D and the length of exposure. Vitamin D toxicity may include vomiting, loss of appetite, increased thirst, increased urination, and excessive drooling to renal (kidney) dysfunction.
Purina is taking this action after receiving two contacts about two separate confirmed cases of a dog exhibiting signs of vitamin D toxicity after consuming the diet, to date. Once taken off the diet, each of these dogs recovered.
The affected dry dog food was distributed throughout the United States by prescription only through veterinary clinics, Purina Vet Direct, Purina for Professionals, and other select retailers with the ability to validate a prescription.
Bags of PPVD EL with the UPC Code and Production Code below should be immediately discarded.
| Product | UPC Code | Production Code (*First 8 characters equal to) |
|---|---|---|
| Purina Pro Plan Veterinary Diets EL Elemental (PPVD EL) 8 lb and 20 lb bags |
38100 19190 – 8 lb 38100 19192 – 20 lb |
2249 1082 2250 1082 2276 1082 2277 1082 2290 1082 2360 1082 2361 1082 |
Pet owners who purchased bags of the product listed above are asked to immediately stop feeding and throw it away in a container where no other animals, including wildlife, can get to it. If signs such as weight loss, excessive drooling, vomiting, loss of appetite or increased thirst or urination have occurred in their dog while eating this diet, pet owners should contact their veterinarian.
No other Purina pet care products are affected.
Veterinary and other retail partners should remove and destroy the affected product from their inventory.
We apologize to pet owners and veterinarians for any concerns or inconvenience this situation has caused. As pet experts and pet owners ourselves, the health and well-being of pets is our top priority.
Please contact our team directly Monday – Saturday, 8am – 5pm CST at 1-800-345-5678 or via email at https://www.purina.com/contact- usExternal Link Disclaimer for questions or assistance in getting a refund.
Company Contact Information
Consumers:Purina 1-800-345-5678
Product Photos
Warning signs and treatment for Poodle Glaucoma

A standard poodle is a beautiful addition to your family. They are considered child-friendly and loyal companions. Whether you own a poodle or have the option of adopting the perfect pup into your home, researching medical history for inherited conditions is very important. Knowing what risk factors and symptoms to watch for in a disease like glaucoma is crucial to reducing the onset of symptoms. Remember that purebred dogs are more likely to suffer from diseases and other medical conditions. Therefore, being a responsible pet owner might look like investing in pet health insurance. This type of insurance will give you a security blanket to optimize medical procedures to reduce pain and damage.
To find out more about glaucoma in poodles, Breed Expert has a great article
Recalls
Voluntary Recall of Northwest Naturals Brand 2lb Feline Turkey Recipe Raw Frozen Pet Food
Due to HPAI Contamination
Portland, Oregon, Northwest Naturals is voluntarily recalling one batch of Northwest Naturals brand 2lb Feline Turkey Recipe raw frozen pet food after it was tested positive for highly pathogenic avian influenza (HPAI) virus.
Consumption of raw or uncooked pet food contaminated with HPAI can cause illness in animals. To date, one case of illness in a domestic cat has been reported in connection with this issue.
The recalled product is packaged in 2-pound plastic bags with “Best if used by” dates of 05/21/26 B10 and 06/23/2026 B1. The product was sold through distributors in AZ, CA, CO, FL, GA, IL, MD, MI, MN, PA, RI and WA in the United States, and British Columbia in Canada.
This recall is being conducted in cooperation with the Oregon Department of Agriculture, Salem, Oregon.
Consumers who have purchased the recalled product should immediately discard the product and contact the place of purchase for a full refund.
For additional information or questions, customers may contact Northwest Naturals of Portland at info@nw-naturals.net or 866-637-1872 from 7:00 AM to 3:30 PM PST, Monday through Friday.


Northwest Naturals recall notice: https://www.nw-naturals.net/12-24-24-voluntary-product-recall/
Angel Fund, SPCA Team up to Help Male Cat With Bladder Problem

Luis Hernandez felt pretty much at the end of his rope one day last August. He was unemployed and his beloved cat Gordo appeared to be in major trouble. The animal was in pain and bleeding 10 days after having a third surgery to clear a bladder blockage that had cost the last of Luis’s dwindling savings.
“I was in a pretty desperate state,” he said. “I had gone one last time to the veterinary clinic where I had been going for some time and I was begging them for some help. I was literally saying: ‘Look, you have all my money. I just gave it all to you. There’s no more money. Please help me make a decision.’
“Gordo had started bleeding soon after that last surgery and it was pretty bad,” Luis said.
And, on top of his concern for his nine-year old cat, he was annoyed by a poster in the clinic’s lobby advertising PU (perineal urethrostomy) surgery that could create a new urinary opening that might decrease the likelihood of recurring urinary obstruction. “Is it right for your cat?” the poster asked. Gordo fit the description of a cat that would benefit from the surgery.
If the hospital had told him about the surgery earlier, he said, he would have had it done – when he had the money to pay for it.
“I was there begging for help with guidance on what to do to help Gordo. Did they think my cat had kidney damage from his three blockages? And why is he bleeding? So I left that day with my cat in my arms and I called the SPCA and asked them for assistance.
“The folks at SPCA were very kind over the phone,” Luis said. “They cared about my situation and they were trying to find a place where I could get care free of charge. I told them I couldn’t afford to take him to the hospital any more and that he was suffering.”
The SPCA made an appointment for Gordo at Berkley Veterinary Clinic in North Hollywood. Luis took his cat there that same day. He saw Dr. Jinny Park, who owns the practice. He told her what had happened. She asked if he had considered the PU surgery. “I told her that I had just recently found out about that surgery and that I was not in position to afford it.”
Dr Park, he said, “was very compassionate and she understood my situation. And she said: ‘If possible I could get some funds from Angel Fund and maybe the SPCA. And if that could happen, I will cover the remaining cost of the surgery for Gordo. It will be free for you.’
“I was pretty shocked at her generosity and compassion. It was pretty hard to fight back my tears. It was a pretty crazy moment there. I told her, ‘Yeah, I would love that and I would be super grateful if you could do that.’”
Dr. Park called Luis later that day and told him that she had contacted Angel Fund and the SPCA and that the funds had been made available. He took Gordo in the next morning for the surgery. Luis picked up his pet a day later.
The Berkley staff had rallied behind Gordo and “they were really pushing for his success,” Luis said. “It was really great to see.” Gordo went home with a cone that he would wear for a week.
“I felt great relief knowing that he was going to get better and not be in so much pain. And once he started using his litter box the way he normally did – it was a relief to see that happen.”
He expressed gratitude for the financial help that he received from Angel Fund and the SPCA. He said that he told several of his friends about his experience and four of them said they planned to take their pets to Dr. Park in the future.
Luis still faces some struggles but having a healthy Gordo has had a positive influence on his life in a difficult time. His “housing situation has been rocky at times the last couple of years,” he said. But he does do some part-time work, he has a girlfriend he loves and he is hopeful about his future.
PTSD and Service Dogs
Veteran Statistics & Resources
PTSD Service Dogs, Between Statistics and Veterans’ Voices
PTSD Service Dogs, Between Statistics and Veterans’ Voices
Table of Contents
- An Emerging Complementary Treatment
- Veterans’ Voices: Interest in PTSD Service Dogs
- Recent Research Shows the Benefits of PTSD Service Dogs
- PTSD Service Dogs vs. Emotional Support Dogs
- Specific Tasks Performed by Service Dogs
- In Veterans’ Own Words
- Conclusion
- References
While service dogs have traditionally been provided to assist veterans with physical disabilities, there has been a growing interest in using service dogs to improve the quality of life of veterans suffering from mental health disorders. This article will explore some of the most recent research on the impact of service dogs in the treatment of PTSD.
An Emerging Complementary Treatment
Although PTSD awareness and treatments greatly improved in recent decades, U.S. military personnel have been encountering unprecedented stressors, resulting in an elevated risk of developing PTSD. Soldiers who served in Operations Iraqi Freedom (OIF) and Enduring Freedom (OEF) were exposed to the constant threat of improvised explosive devices (IEDs) and the strain of multiple deployments. These warfare conditions have contributed to PTSD cases that are often more severe than those observed following the Vietnam War.
29% of Iraqi Freedom and Enduring Freedom veterans develop PTSD.
2024
U.S. Department of Veterans Affairs
A 2015 meta-analysis of the studies involving OEF/OIF veterans estimated that approximately 23% of veterans who served in Iraq and Afghanistan had PTSD [1]. The current estimate recognized by the U.S. Department of Veterans Affairs (VA) is a 29% PTSD rate for the veterans who participated in the operations Iraqi Freedom and Enduring Freedom. Consequently, the demand for effective PTSD treatments for veterans has remained high, possibly surpassing that of any previous era in U.S. military history.
The VA has been providing a range of psychotherapies for PTSD treatment that can be broadly classified into two categories: trauma-focused and non-trauma-focused therapies. Trauma-focused therapies directly address traumatic experiences, requiring patients to actively engage with trauma-related memories, beliefs, and triggers. These therapies utilize various strategies, including behavioral, cognitive-behavioral, and emotion-focused approaches. In contrast, non-trauma-focused therapies avoid direct engagement with traumatic events, instead concentrating on building support, empathy, insight, and adaptive coping mechanisms.
Research has consistently demonstrated that trauma-focused therapies are significantly more effective. Therefore, the VA primarily offers two trauma-focused psychotherapies: Prolonged Exposure (PE) and Cognitive Processing Therapy (CPT). These treatments have a remarkable efficacy in reducing PTSD symptoms and have benefited many veterans. However, their effectiveness hinges on the patient’s consistent and active participation over an extended period, often involving emotionally and practically demanding tasks. Such high level of commitment poses a persistent challenge for many veterans engaging in PE and CPT. [2]
Analysis of recent studies has shown that trauma-focused treatments have an average dropout rate of 27.1% among enlisted service members [3]. This could be even higher in uncontrolled conditions. Maguen et al.’s (2019) research of a single Veteran’s Health Administration facility under typical conditions, spanning from October 2001 to September 2015, found that only 22.8% of veterans initiated evidence-based psychotherapies like PE or CPT [4]. More concerningly, a mere 9.1% of this group completed the treatment, translating to an attrition rate exceeding 60%.
Recent research has explored the potential of non-trauma focused interventions that encourage patient engagement and retention while addressing PTSD symptoms. One promising adjunct intervention is the use of specially trained psychiatric service dogs. These dogs are distinct from emotional support, therapy, or companion animals in that they are specifically trained to perform tasks tailored to the psychiatric needs of their handlers, such as interrupting anxiety episodes, waking them from nightmares, or providing a buffer in crowded public settings.
Note: the VA does not currently provide or support service dogs for mental health conditions, including PTSD, and is still studying the potential benefits of such interventions.
Veterans’ Voices: Interest in PTSD Service Dogs
In August 2024, Hill & Ponton polled its audience to gauge the level of interest and access to PTSD service dogs. The 678 veterans who answered provide a snapshot of the current landscape regarding PTSD service dogs:
- 8.25% have at some point had a PTSD service dog
- 2.80% applied to get one but didn’t get it or are still waiting
- 44.39% never had one but would like a PTSD service dog
- 19.32% don’t want or need one
- 25.22% don’t know enough about PTSD service dogs
The answers suggest that there is significant interest among veterans for PTSD service dogs, coupled with a lack of access. Moreover, a quarter of those polled lacked information about this type of treatment.

Comments received from Veterans include:
A private psychologist did testing to support my PTSD claim and recommended that I get a service dog to help me deal with PTSD issues. Archie has been my angel service dog, and truly helps me daily living with PTSD and migraines.
A social worker said a service dog would benefit me but that was a couple years ago, and nothing has been said to me since then.
My personal dog goes everywhere possible with me and can tell when I’m getting uncomfortable. He will get on my lap, paw at me, get my attention. I would love to get him trained and certified to travel with me more places. Would love to get more info on the subject.
I don’t know how to even begin to seek receiving a service dog.
I attended several nonprofit organizations that provide PTSD Service dogs to veterans without success as the dogs were not properly trained. I purchased my own puppy and paid to acquire great training from a for profit organization. My dog is now trained for mobility, PTSD, scent detection, tracking and personal security. She is better than any dog I could get from a non profit for PTSD. Alot of it is because I put skin in the game and was totally committed. I am training another puppy for when my current service dog retires.
Recent Research Shows the Benefits of PTSD Service Dogs
Multiple studies utilizing the PTSD Checklist (PCL), a standardized self-report scale, have found that being partnered with a service dog is associated with significantly lower PTSD symptom severity compared to not having a service dog.
Rodriguez et al. (2018) compared 45 veterans with service dogs to 28 on a waitlist and found those with dogs scored significantly lower on the PCL. [5]
Most recently, Leighton et al. 2024 nonrandomized controlled trial of 156 veterans and military members [6], which is the largest nationwide study to date to compare the use of PTSD service dogs with usual care alone, measured PTSD symptoms after 3 months, with the following results:
The PCL-5 test
- Service dog group average score: 41.9
- Control group average score: 51.7
The CAPS-5 test
- Service dog group average score: 30.2
- Control group average score: 36.9
The service dog group’s lower scores represent significantly lower PTSD symptom severity. The researchers also looked at how many people still met the criteria for PTSD after 3 months:
- In the service dog group, 75% (51 people) still had PTSD
- In the control group, 85% (56 people) still had PTSD
Beyond subjective self-report measures, biological markers also point to the therapeutic effects of service dogs. Rodriguez et al. (2018) examined the cortisol awakening response (CAR) in veterans with and without service dogs. The study found that veterans with service dogs had a bigger morning spike in cortisol compared to those without, which would indicate a healthier response to stress. This biological evidence supports the notion that service dogs may help restore balance to veterans’ stress response systems.
In 2024 a 3 month clinical trial drew similar conclusions, suggesting that service dog placement could help boost veterans’ morning cortisol response. [7]
These consistent findings across multiple studies provide strong evidence for the efficacy of service dogs in reducing PTSD symptom severity among veterans.
PTSD Service Dogs vs. Emotional Support Dogs
The Richerson et al. (2023) study, titled “Therapeutic and Economic Benefits of Service Dogs Versus Emotional Support Dogs for Veterans With PTSD,” [8] is one of the most comprehensive investigations to date. The researchers conducted a multicenter trial with 227 veterans with PTSD over 18 months, randomly assigning them to receive either a service dog or an emotional support dog.
Results:
PTSD Symptoms: Participants with service dogs had a 3.7-point greater reduction in PTSD symptoms compared to those with emotional support dogs.
Medication Adherence: Veterans with service dogs had an increase of 10 percentage points in antidepressant adherence compared with those with emotional support dogs.
This study provides strong evidence for the specific benefits of service dogs over emotional support dogs in reducing PTSD symptoms and improving medication adherence.
Specific Tasks Performed by Service Dogs
To understand how service dogs alleviate PTSD symptoms, Rodriguez et al. (2020) surveyed a group of veterans’ perceived importance of the trained tasks performed by service dogs:
- Interrupt/alert – The dog lets the veteran know when they are feeling anxious and interrupts with a nose bump, placing head in lap, or some other behavior.
- Calm/comfort anxiety – The dog performs a calming behavior such as making physical contact (laying on top of handler, placing head in lap, gently leaning against the body) when the veteran feels distress or anxiety.
- Block (create space) – The dog positions itself horizontally in front of the veteran to create personal space.
- Block (guard/protect) – The dog positions itself horizontally in front of veteran to guard/protect.
- Cover (watch back) – Dog positions itself directly behind the veteran to “watch” the veteran’s back.
- Social greeting – The dog helps greet people in public by sitting/offering a paw.
- Wake up from nightmare – The dog recognizes that the veteran is having a nightmare and gently wakes them up.
The study found that the task most frequently performed by service dogs was to calm/comfort anxiety, reported in 52% of daily check-ins. [9] The “cover” or “watch my back” task was the second most frequently used, averaging 4.1 times daily. This task mimics military camaraderie, where soldiers guard each other’s blind spots in combat. Veterans report that this helps them share the burden of being constantly alert in public.
The social greeting task, while less broadly applicable to PTSD symptoms, was still considered moderately important. It’s especially useful in public interactions and may contribute to reduced social isolation and increased participation observed in veterans with service dogs.
The nightmare wake-up task specifically targets intrusive memories, nightmares, and sleep disturbances. 57% of veterans found this helpful for trauma-related nightmares, making it a crucial aspect of the service dog intervention for many.
The two versions of the “block” task – creating personal space and guarding/protecting – were rated similarly by veterans. While some mental health professionals worry this task might reinforce avoidance behaviors, veterans found it moderately to quite important for their PTSD.
Overall, service dog tasks addressed almost every DSM-5 PTSD symptom, with intrusion symptoms benefiting from the most tasks, particularly calm/comfort and interrupt/alert. The dogs’ calming presence and interrupting behaviors appear to help ground veterans during flashbacks and provide relief from distress.
In Veterans’ Own Words
The most helpful thing the dog does for one veteran is to “be able to walk through life knowing that if I were to have an anxiety attack it wouldn’t be the end of the world, I would have my battle buddy [service dog] to get through it.” [10]
For others, a service dog:
- “reminds me to take my medication because he senses my mood and work [quality] deteriorates if I don’t take my medication. “
- “gets me motivated, to get up and get outside” [11]
- “[gives] constant companionship, I know he is always by my side. We are always together.”
- “sleeps with me and wakes me up from nightmares”
- “has allowed me to go to crowded public places to support my children’s activities that I previously would not have gone to”
- “blocks people from getting too close and forces me to focus on her when I have rage episodes”
- “has allowed me to become the father and husband I am supposed to be”
- “has definitely improved my life in so many ways and has given me a better outlook overall” [10]
For these veterans, service dogs are more than just a treatment option. Their unconditional love and devoted companionship sets service dogs apart from other interventions and enables profound transformation of veterans’ lives.
Conclusion
The use of service dogs for veterans with PTSD shows promise as a complementary intervention. Current evidence suggests that service dogs can contribute to reduced PTSD symptoms and enhanced social functioning for many veterans. The high level of interest in PTSD service dogs among veterans underscores the need for continued research, education, and support.
References
- Fulton, J.J.; Calhoun, P.S.; Wagner, H.R.; Schry, A.R.; Hair, L.P.; Feeling, N.; Elbogen, E.; Beckham, J.C. The prevalence of posttraumatic stress disorder in Operation Enduring Freedom/Operation Iraqi Freedom (OEF/OIF) veterans: A meta-analysis. J. Anxiety Disord. 2015, 31, 98–107. https://www.sciencedirect.com/science/article/abs/pii/S0887618515000262
- Lee, A.J.; LaFreniere, L.S. Addressing Attrition from Psychotherapy for PTSD in the U.S. Department of Veterans Affairs. Trauma Care 2023, 3, 274-293 https://www.mdpi.com/2673-866X/3/4/24
- Edwards-Stewart, A.; Smolenski, D.J.; Bush, N.E.; Cyr, B.-A.; Beech, E.H.; Skopp, N.A.; Belsher, B.E. Posttraumatic stress disorder treatment dropout among military and veteran populations: A systematic review and meta-analysis. J. Trauma. Stress 2021, 34, 808–818. https://pubmed.ncbi.nlm.nih.gov/33524199/
- Maguen, S.; Li, Y.; Madden, E.; Seal, K.H.; Neylan, T.C.; Patterson, O.V.; DuVall, S.L.; Lujan, C.; Shiner, B. Factors associated with completing evidence-based psychotherapy for PTSD among veterans in a national healthcare system. Psychiatry Res. 2019, 274, 112–128. https://pubmed.ncbi.nlm.nih.gov/30784780/
- O’Haire, M. E. & Rodriguez, K. E. Preliminary efficacy of service dogs as a complementary treatment for posttraumatic stress disorder in military members and veterans. J. Consult. Clin. Psychol. 86, 179–188 (2018). https://pubmed.ncbi.nlm.nih.gov/29369663/
- Leighton SC, Rodriguez KE, Jensen CL, et al. Service Dogs for Veterans and Military Members With Posttraumatic Stress Disorder: A Nonrandomized Controlled Trial. JAMA Netw Open. 2024;7(6):e2414686 https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2819452
- Nieforth LO, Rodriguez KE, Zhuang R, et al. The cortisol awakening response in a 3 month clinical trial of service dogs for veterans with posttraumatic stress disorder. Sci Rep. 2024;14(1):1664 https://pubmed.ncbi.nlm.nih.gov/38238350/
- Richerson JT, Wagner TH, Abrams T, et al. Therapeutic and economic benefits of service dogs versus emotional support dogs for veterans with PTSD. Psychiatr Serv. 2023;74(8):790-800 https://pubmed.ncbi.nlm.nih.gov/36718602/
- Rodriguez KE, LaFollette MR, Hediger K, Ogata N, O’Haire ME. Defining the PTSD Service Dog Intervention: Perceived Importance, Usage, and Symptom Specificity of Psychiatric Service Dogs for Military Veterans. Front Psychol. 2020 Jul 21;11:1638. https://pubmed.ncbi.nlm.nih.gov/32849004/
- Nieforth LO, Rodriguez KE, O’Haire ME. Expectations versus experiences of veterans with posttraumatic stress disorder (PTSD) service dogs: An inductive conventional content analysis. Psychol Trauma. 2022 Mar;14(3):347-356 https://pubmed.ncbi.nlm.nih.gov/33630635/
- Crowe, T. K., Nguyen, M. T., Tryon, B. G., Barger, S., & Sanchez, V. (2018). How Service Dogs Enhance Veterans’ Occupational Performance in the Home: A Qualitative Perspective. The Open Journal of Occupational Therapy, 6(3). https://scholarworks.wmich.edu/ojot/vol6/iss3/12/
Pea Sensitivity in Dogs and Cats

September 29, 2024 / Nutrition / By W. Jean Dodds

High legume content in grain-free commercial dog foods – particularly peas and lentils – were implicated as possibly causing dilated cardiomyopathy (DCM) in dogs by the Food and Drug Administration (FDA). The FDA has since pretty much retracted that statement.
DCM is a form of heart disease. This post is about pea sensitivity or intolerance – an immunological response – that could possibly cause itchy skin or upset stomachs.
Commercial pet food manufacturers add peas or pea fiber to dog and cat food. Several reasons exist for this addition.
- Peas are used instead of white potatoes which rank high on the glycemic index and can also cause immunological reactions in certain pets.
- Peas and pea fiber have a binding quality similar to potatoes that is necessary for kibble.
Cross-Reactivity of Peas
Peas are legumes and a part of the Fabaceae (Leguminosae) family and which includes soy, peanuts, chick peas, and lentils. The allergens contained in peas are closely related to, or found in, other legumes. Several clinical studies have been conducted around the world to find out if humans known to have a sensitivity to one legume will have a similar sensitivity to another. While my immunology peers debate the significance, it has been proven that some people will have cross-reactivity – not everyone does, but a decent percentage do.
NutriScan, Hemopet’s patented pet food sensitivity and intolerance test, measures a dog or cat’s saliva for IgA and IgM reactions to lentils, peanuts, and soy, along with other ingredients. So, it is my advice that if the results suggest that you avoid one of these three, it would be best to avoid peas as well.
It may appear a stretch to apply human results to dogs, but remember that the University of Chicago and other international institutions found that humans and domestic dogs share an extensive parallel genomic evolution, particularly in genes associated with digestion and metabolism, neurological processes and diseases such as cancer. According to the researchers, these genes have likely evolved in parallel due to the close living environment shared by humans and dogs over many thousands of years, including possibly scavenging for food together.
Conclusion
Unfortunately, pet food manufacturers recognize sensitivity reactions to meat-proteins, grains, and potatoes but typically are not concerned about or are unaware of the similar impact of other ingredients. So, they will use peas as a standardized product in limited ingredient foods. While I applaud the introduction of limited ingredient foods, I urge them to expand their product options. This is a significant reason why I prefer home-cooked meals for pets.
Dodds, Jean, DVM, and Diana Laverdure, MS. Canine Nutrigenomics: The New Science of Feeding Your Dog for Optimum Health. DogWise Publications, Wenatchee, WA, 2015. Print.
“Pea.” Phadia. N.p., n.d. http://www.phadia.com/en/Products/Allergy-testing-products/ImmunoCAP-Allergen-Information/Food-of-Plant-Origin/Legumes/Pea-/.
“Peanut and Green Pea Possible Allergy.” Peanut and Green Pea Possible Allergy. AAAAI, 28 Oct. 201. http://www.aaaai.org/ask-the-expert/peanut-pea-allergy.aspx.
Originally Published: May 17, 2015
Updated: May 22, 2024
S
AHF Angel Fund Helps Cheeto, Tabby with Blocked Bladder


One day a few weeks ago, Ashley Bettencourt came home from her job as a pre-school teacher and found her tabby cat Cheeto in distress.
“He wasn’t himself,” she said. “He wasn’t eating. He was lethargic and was lying on the tile in the hallway. He wasn’t moving. Nothing worked that I knew would make him excited.
“I thought maybe he was constipated but I pressed on his belly and it was really hard. It made me nervous. So I called the Cat Care Clinic where my in-laws take their cats. After taking him in for an examination, I was told that he had a blocked bladder – he wasn’t able to urinate.”
That was on a Friday. Dr. Maggie Mills treated Cheeto. “They didn’t have to do surgery but they kept him in the hospital the whole weekend so they could keep an eye on him,” Ashley said. “They put in a catheter. But they said he took it out himself. So they put the tubes back in and he didn’t fight them again.
“When I took him in to the clinic, I wasn’t expecting what was coming,” she said. “I thought he was constipated and they would fix it and I would take him home. So when it came time to pay I was like, ‘I can’t do this.’
But the staff at Cat Care was understanding and helpful. April, the assistant practice manager, “was so sweet and nice,” Ashley said. “She printed me out a list of foundations that could help and she pointed out who to call and told me what to do. Angel Fund was the first to say, ‘We’ll help you.’ I had never done something like that before. It was overwhelming in a good way.
“I went home and I cried that night. I thought what happened was amazing. I couldn’t believe it.” She said that she found another charitable group that helped pay her bill. And the Cat Care Clinic found some money from another fund and they used that to help as well, she said.
“They said (at Cat Care) that, if we couldn’t do this, they would have had to euthanize Cheeto. He always had been such a healthy cat that is horrible to even think about. I love that Angel Fund and the veterinary association are letting people know about this. I wouldn’t have known if it wasn’t for Dr. Mills and April.”
Cheeto recovered quickly. “Now, he is good, he’s happy,” Ashley said. “He’s lost a lot of weight. But he’s eating well. He’s drinking a lot of water. And he’s fine, he’s active and he’s playing with our other cats.”
Cheeto is the father of the other cats, Roxy, Khola Man and Sprinkles – all named by Ashley’s daughters. There is also a dog in the family, Benny a miniature Doberman, with whom Cheeto is a best buddy. “We are a house that loves our fur babies,” Ashley said.
Cheeto became a member of the family after Ashley’s husband found him hiding among tires at the warehouse where he worked. He was a three-week-old kitten at the time and had to be bottle fed.
Ashley is a single parent to three daughters: Bella, 13; Skylar, 11 and Audrina, 7. She loves her job as a pre-school teacher. “It’s challenging but I love it. my students are four and five. They talk fast but they’re willing to learn and they love it.”
Vaccine Titer Testing for Dogs and Cats
September 8, 2024
Infectious Diseases & Vaccines / By Dodds

Over the past few years, we have seen serological titer testing partially embraced by major veterinary associations to discover if a companion dog or cat is immunized against a particular infectious disease.
Before we get into the debate of titer testing, let’s discuss the basics.
What is a titer test?
A titer test is a simple blood test that measures an animal’s antibodies to viruses or other infectious agents.
What is the difference between sterilizing immunity and non-sterilizing immunity?
Basics
Sterilizing immunity = prevents clinical disease and protects from infection. The vaccines: canine distemper, parvovirus, adenovirus-2 (covers hepatitis); and, feline panleukopenia (a parvovirus) produce sterilizing immunity.
Non-Sterilizing immunity = does not protect against infection; but should keep infection from progressing to severe clinical illness. Examples of vaccines that produce non-sterile immunity would be leptospirosis, Bordetella, rabies virus, influenza, herpesvirus and calicivirus – the latter two being upper respiratory viruses of cats.
Discussion
As previously stated, sterilizing immunity not only prevents clinical disease but also prevents infection, and only the presence of antibody can prevent infection. As stated by the late eminent expert Dr. Ronald Schultz in discussing the value of vaccine titer testing, these tests “show that an animal with a positive test has sterilizing immunity and should be protected from infection.”
The vaccines that do provide sterilizing immunity are distemper virus, adenovirus, and parvovirus in the dog, and panleukopenia (feline parvovirus) virus in the cat.
While non-sterile immunity may not protect the animal from infection, it should keep the infection from progressing to severe clinical disease.
Why titer test?
- History of Adverse Events to Vaccinations
- Vaccinosis – Dogs and cats with immune-mediated diseases or predisposed to them are especially vulnerable to vaccinosis, since over-vaccination places additional stress on their already compromised immune systems and has been linked to autoimmune disease.
- Sterilizing Immunity – An animal with a positive test to the sterilizing vaccines should be protected from infection. If that animal were vaccinated it would not respond with a significant increase in antibody titer, but may develop a hypersensitivity to vaccine components (e.g. fetal bovine serum and the excipients). Furthermore, the animal doesn’t need to be revaccinated and should not be revaccinated since the vaccine could cause an adverse reaction.
Testing
Serological antibody titer testing has become more readily available over the past several years with veterinary reference laboratory and the availability of in-house testing kits. While this in-house testing is convenient, the gold standard is still laboratory testing because several of the available kits have been documented to vary in accuracy.
Interpreting Titer Results
Research has shown that once an animal’s titer stabilizes to sterilizing vaccines or infections, it is likely to remain constant for many years. It is often said that the antibody level detected is “only a snapshot in time”. That’s simply not true; it is more a “motion picture that plays for years”.
Protection – as indicated by a positive titer result – is not likely to suddenly drop-off unless an animal develops a medical problem such as cancer or receives high or prolonged doses of immunosuppressive drugs. Viral vaccines prompt an immune response that lasts much longer than that elicited by classic antigen. Lack of distinction between the two kinds of responses may be why practitioners think titers can suddenly disappear.
In all actuality, interpreting titers correctly depends upon the disease in question and if the vaccine produces sterilizing or non-sterilizing immunity. Some titers must reach a certain level to indicate immunity, but with other agents like those that produce sterile immunity, the presence of any measurable antibody shows protection.
The positive titer test result is fairly straightforward, but a negative titer test result is more difficult to interpret, because a negative titer is not the same thing as a zero titer and it doesn’t necessarily mean that animal is unprotected. Indeed, one of the drawbacks of titer testing is that it does not measure cellular immunity. Anyway, a negative titer result usually means the titer has failed to reach the threshold of providing sterile immunity.
This is an important distinction, because for the clinically important distemper and parvovirus diseases of dogs and panleukopenia of cats, a negative or zero antibody titer indicates that the animal is not protected against canine parvovirus and may not be protected against canine distemper virus or feline panleukopenia virus. While non-sterile immunity may not protect the animal from infection, it should keep the infection from progressing to severe clinical disease.
Puppy Recommendations
Since 2016, the World Small Animal Veterinary Association (WSAVA) Vaccination Guidelines have partially embraced serological titer testing for canine distemper (CDV), parvovirus (CPV), and adenovirus (CAV) for puppies. For kittens, the guidelines mention titer testing for antibodies against feline panleukopenia (a parvovirus), but it is not discussed to the degree that puppy titer testing is.
In a snapshot, the WSAVA states that a companion pet caregiver can choose to have their puppy titer tested for those three diseases four or more weeks after the final set of initial vaccinations. If a puppy has a positive test result, the puppy does not need to be revaccinated for another three years. If they choose not to titer test, WSAVA recommends vaccinating once more at 26 weeks and then three years after that.
For instance, the association suggests the last set of puppy vaccinations against CDV, CPV, and CAV-2 (covers ICH = CAV-1) be given at 16 weeks. At 20-26 weeks of age, titer test or opt for a final vaccination at 26 weeks.
One of the key points WSAVA emphasizes is that laboratory testing is the gold standard for serological titer testing and is much preferred over the in-house tests – particularly for CDV and CAV.
Dog and Cat Recommendations
For years, the WSAVA has recommended triennial vaccinations of core vaccines: canine distemper, parvovirus, and adenovirus-2 (covers infectious canine hepatitis/ICH); and feline panleukopenia (a parvovirus) after the initial vaccination series given to puppies and kittens.
We applaud this recommendation because it essentially extended the interval from one year to every three. However, we think it fails to include a valid step: titer testing.
Indeed, we prefer that individual dogs and cats be titer tested every three years to determine if they do in fact need this vaccination after the initial vaccination series given to puppies and kittens.
The AAHA Stance
In contrast to WSAVA, AAHA does not embrace titer testing…except in certain instances.
The AAHA Canine Vaccination Guidelines of 2022 discuss the drawbacks of titer testing such as: interpretation; differences between the various laboratories and the results they output; issues with in-house testing; lack of new research; and, questions of the test’s validity. The Association has stated, “It can be misleading to forecast an outcome on the basis of one cofactor: a titer.”
Yet, AAHA’s triennial vaccination protocol for feline panleukopenia, canine distemper, canine parvovirus, and canine adenovirus-2 is based on titer testing.
Further, while the Association does not advise to routinely rely on or use titer testing, it does provide exceptions, “except in cases in which dogs have a history of adverse responses to vaccination, there is a suspicion of vaccine-related autoimmune disease, or when owners express resistance or hesitancy to having their dogs vaccinated or boostered—in which case client communication and education may help overcome this hesitancy.”
They appear to be equivocating.
Reminder
Dr. Dodds still wants puppies properly vaccinated against canine distemper and parvovirus, and cats against feline parvovirus (panleukopenia). Remember: more often than not, these diseases are worse than the vaccinations against them! We want to immunize wisely and not overly vaccinate. That’s why we advocate for laboratory titer testing, which is a service Hemopet provides.
From AP: Giving up pets to seek rehab can worsen trauma. A Colorado group intends to end that
For many people entering rehab, the inability to find someone to care for their pets while they are away is often difficult and painful. An organization in Colorado called PAWsitive Recovery has stepped up to help fill that void by taking care of pets for people going through treatment for drug and alcohol abuse. (AP video by Thomas Peipert)
2 of 5 |
Simon Rubick, who sought help from PAWsitive Recovery while he was recovering from drug and alcohol addiction, holds his rescue dog Tonks in Aurora, Colo., on Monday, June 3, 2024. (AP Photo/Thomas Peipert)
3 of 5 |
Simon Rubick, who sought help from PAWsitive Recovery while he was recovering from drug and alcohol addiction, holds his rescue dog Tonks in Aurora, Colo., on Monday, June 3, 2024. (AP Photo/Thomas Peipert)
4 of 5 |
Ben Cochell, a volunteer for PAWsitive Recovery, lets his foster dog Dexter lick his face at his home in Denver on Tuesday, March 26, 2024. (AP Photo/Thomas Peipert)
5 of 5 |
=Ben Cochell, a volunteer for PAWsitive Recovery, walks his foster dog Dexter with his family in Denver on Tuesday, March 26, 2024. (AP Photo/Thomas Peipert)
By THOMAS PEIPERTUpdated 8:39 AM PDT, September 1, 2024Share
DENVER (AP) — Simon Rubick had lost almost everything to decades of alcoholism and drug addiction.
In 2022, he found himself without a vehicle and without a home, which forced his two teenage children to move in with friends. He had burned bridges with friends and family and it took a drug-induced stint in the hospital for him to realize his cocaine addiction was going to be a “death sentence.”
Rubick, who lives in the Denver suburb of Arvada, Colorado, knew he needed help. But first he had to figure out what to do with one of the only sources of unconditional love and support he had left: his beloved German shepherd rescue, Tonks.
Most residential rehab centers in the United States don’t allow patients to bring their pets along, said Rubick, 51. So when his brother could no longer help care for the dog, Rubick thought he would have to make the excruciating decision to give up Tonks.
“It basically came down to being able to take care of my dog or being able to take care of myself,” he said.
Rubick — who has been sober for more than two years and is now an addiction recovery coach — was connected to the group PAWsitive Recovery, which fosters animals while their owners receive treatment for drug and alcohol abuse, and for people dealing with domestic violence or mental health crises.
“People that are trying to get into recovery sometimes have lost their families, their children, any kind of support system that they have had,” said Serena Saunders, the organization’s program manager. “You’re not going to compound trauma that you’ve already had by giving up the one thing that hasn’t given up on you, and that’s people’s animals.”
Saunders founded PAWsitive Recovery in Denver three years ago. Since then, it’s helped more than 180 people and their pets, and Saunders said the group has looked to expand nationally after it became a part of the Society for the Prevention of Cruelty to Animals International. The organization, whose largest foster network is in Colorado but accepts applications nationwide, is one of just a few programs in the U.S. that cares for the pets of people seeking treatment for substance abuse.
Saunders’ own experience with drug and alcohol addiction has helped her tailor the program. She said she had a “pretty broken childhood,” with her mother being schizophrenic and addicted to methamphetamine and her father also struggling with addiction. She sought comfort in alcohol when she was about 12 and was using hard drugs by the time she was 14.
“Addiction just gave me trauma after trauma,” said Saunders, now 41.
Saunders was seeing a therapist for her depression and PTSD when a fortuitous session planted the seed of PAWsitive Recovery. With a background in veterinary and shelter medicine, which focuses on caring for homeless animals, she told her therapist she wanted to incorporate her love of dogs in her recovery.
“And that’s what we did,” said Saunders, who fostered Tonks for several months while Rubick was in treatment and facilitated visits between the two best friends.
“To see a broken person when we’re meeting them in a parking lot, when they have nothing left to live for but their animal. And to see how broken and how desperate they are in that moment, and then to circle back around six months later and see them completely turn their lives around is just so special. It’s amazing,” said Saunders, who has been sober for 3 1/2 years.
That sentiment is echoed by the organization’s volunteer foster families, some of whom are drawn to the program because of their own experiences with addiction.
Denver resident Ben Cochell, 41, who has been sober from alcohol for more than seven years, has two dogs of his own and has fostered several more.
“One of my favorite parts about fostering in this program is the ability to teach my kids some life lessons in how to help others and how to care for animals and be kind, be loving. And to just give of yourself,” he said. “That’s what you have. Your time and your energy. And you can give that away freely.”
If not for PAWsitive Recovery, Rubick said he probably would have ended up living on the streets with his dog and trying to figure out recovery on his own. But as it turned out, by being able to keep his rescue dog, Tonks ended up rescuing Rubick, he said.
“It’s that connection, caring for another creature and having something else care for you the way that animals do,” Rubick said. “It’s just unconditional, and sometimes that’s one of the things that people in recovery really need to be able to feel.”
___
Associated Press writer Colleen Slevin contributed to this report.
Helping Your Pet With Separation Anxiety
Prevention is key. And there are a variety of things that can be done to help prevent separation anxiety in pets.
By Texas A&M University College of Veterinary Medicine and Biomedical Sciences
September 4, 2024

If you have ever lived in a household alongside a pet that excessively howls, scratches at the door, or exhibits an overall sense of panic when a loved one leaves the home, it can be beneficial to speak with a veterinarian about the potential diagnosis of separation anxiety.
Dr. Lori Teller, a clinical professor at the Texas A&M College of Veterinary Medicine & Biomedical Sciences, unpacks the actions linked to separation anxiety with methods of how to alleviate the pet’s stress and behavioral responses associated with it.
Unwelcome Changes
Separation anxiety occurs when an animal — most commonly a dog, though some cats may experience this type of anxiety as well — becomes upset due to being apart from their owner or any individual to whom the pet has grown attached.
While anxiety, in general, has many triggers and is frequently multifactorial, Teller said there are specific life-events or experiences that may contribute to a dog’s development of separation anxiety, including:
- Abandonment when young
- Poor socialization, especially when young
- Lack of training to be left alone and to entertain itself
- Divorce of a family member
- Death of a family member
- Sudden change in work or school schedules
According to Teller, a dog’s personality may also contribute to separation anxiety, as some dogs may be naturally more clingy than others.
Stage-Five Clinger
Because anxiety looks different for every pet, it is important to differentiate excitement or a lack of training from anxiety.
Several identifiable canine behaviors that signal separation anxiety are:
- Pacing
- Whining
- Shaking
- Excessive barking, drooling, or panting
- Destructive behavior, including digging out of the yard, or urinating and defecating in the house
Cats also experience stress when there are major changes in their lives or in the household, but they express it differently. Signs that a cat is experiencing separation anxiety may include:
- Urinating in inappropriate locations
- Lack of appetite
- Loud, excessive meowing
If you have concerns about behaviors your pet is displaying, Teller says it’s important to discuss those with your veterinarian. Videos of the behavior can be helpful in determining what is going on.
Prescribed Chill Pills
Teller says treating separation anxiety requires more than a little “chill pill.”
“Medications alone will not resolve separation anxiety,” Teller said. “There are a variety of medications that are used to help alleviate anxiety and make it easier to institute a behavior modification plan.
“Your veterinarian will work with you to create a behavior modification plan to help eliminate undesirable behaviors and replace them with more appropriate ones,” she said.
Another way to help your pet is that when you know a big change is coming, helping them prepare by introducing activities to their routine also may help prevent anxiety when that big change eventually comes.
“Prevention is key, and there are a variety of things that can be done to help prevent separation anxiety in pets,” Teller said. “Pets need to learn that it is OK to be alone and to entertain themselves, even when someone is home.”

Introducing puzzle toys, food-stuffed toys, and long-lasting chews are options that can help to replace that comfort person with a comfort item. And for sense-based comfort, playing the radio and keeping consistent pheromone diffusers in use can create a safe and recognizable space without their favorite human by their side.
According to Teller, another method to potentially reduce anxiety is to encourage your pet to exercise and release some energy prior to leaving for your day at school or work. A long walk or run or game of fetch may do. Through exercise, a dog trades morning stress-filled yelps with a morning nap instead.
Comfort In Confinement
Finally, when dealing with an anxious dog, crates can offer an enclosed sense of security in their distress.
“When putting a dog in a crate, use lots of praise and make sure the dog has a puzzle toy or chew treat when it goes into the crate,” Teller said. “As a dog feels more comfortable, you can gradually increase the amount of space it has access to — moving from the crate to a room and then hopefully to most of the house. It is important that a dog learns from early on that a crate is a safe place. Some dogs may not be amenable to crate training until their separation anxiety has lessened.”
Likewise, cats also need safe places, though usually not crates. These safe spaces can include a room with perches at different levels or nooks where they can hide, Teller says.
“If you notice a change in your dog’s or cat’s behavior, speak with your veterinarian, have a complete physical done, and be sure to let your veterinarian know that there have been changes in the pet’s lifestyle or household,” Teller said.
It is important to recognize that separation anxiety is a medical condition and needs to be treated appropriately. By encouraging your pet’s independence, and working with a veterinarian, as necessary, owners can help instill in their beloved companions behaviors that allow them to thrive on their own.
Julie Ryan Influenced Early In Life by Dr. Joe Cortese

By Jim Bell
When Dr. Julie Ryan-Johnson learned that she had been chosen to receive the Animal Health Foundation’s 2024 Cortese-Lippincott Award, “it was a huge surprise and quite an emotional moment for me,” she said.
That moment took Dr. Ryan back to her first job when, at the age of 11 she worked at the practice of Dr. Joe Cortese. “I knew I wanted to be a veterinarian,” she said. “That’s why I wanted to work for him. I wanted to learn. And he was like a dad to me.”
That also inspired her interest in charitable work “because at the time Dr. Cortese was doing a lot of feral cat spaying and neutering. And one of his clients started an organization to help animals. He was very involved in that.”
The honor also was entirely appropriate for her. The award is presented annually to someone who has “gone above and beyond” to make the world a better place for humans and animals, who excels in community service and education in the veterinary community and who supports the human-animal bond.
Dr. Ryan, who has worked at Boehringer-Ingelheim more than 13 years, runs the shelter and nonprofit programs by providing support of nonprofits with programs involving everything from infectious disease consulting to fund-raising to organizational development.”
It is a job she loves and hopes to continue well into the future. “I really enjoy what I’m doing,” she said. “I love my job. I get to do so much give-back. My company is so supportive and generous with philanthropy.”
Giving back, however, does not stop there, for Dr. Ryan. She also uses her vacation time to do charitable work abroad as well as in the United States. “When I go, I usually go for a week or 10 days. Unfortunately my trips are sometimes determined by disaster situations.” One such trip took her to Poland to help Ukrainian refugees fleeing the Russian invasion in 2022 with their pets.
“I was working with an organization called IFAW – International Foundation of Animal Welfare – through Greater Good Charities,” she said. “Helping pet owners ensure that the animals were healthy enough to take on the next part of their journey was one small thing we could do to help ease their stress and pain. We had helped hydrate, care for travel wounds and then supplied them with everything from pet food to harnesses and leashes. Our tent was open 24/7 with veterinarians and translators.”
Dr. Ryan is the vice chair of Greater Good Charities, and, through the organization, she is able to take such purposeful trips, she said.
The work is rewarding, she said. “It’s wonderful. You’re with a lot of like-minded people who just want to contribute any way they can. These are definitely not glamorous trips – but I love the people I am with.”
Dr. Ryan was nominated for the Cortese-Lippincott Award by Dr. Laura Weatherford and Vivien Flockhart of Boehringer-Ingelheim.
‘The idea for the nomination came from Vivien, who is on the Animal Health Foundation board with me,” Dr. Weatherford said. “Also a co-worker with Julie, Vivien thought she would be a great person to receive the award. But Vivien was busy so I filled out the nomination form based on what she told me and some web searches about Julie.”
Dr. Weatherford said Dr. Ryan was nominated “for all she has done to help people and their pets – and for the greater good of animals.” When she went to Poland to help Ukrainian refugees, Dr. Laura said, “she examined, treated and helped find new homes for pets that owners couldn’t keep.
“She also went to Maui after the 2023 fires to bring donated medications and supplies and to return with several hundred pets from the Maui shelter so there would be room for owned pets on the island.”
Dr Weatherford also noted that – as leader of the BI shelter group – Dr. Ryan helps animal shelters across the country get grants for equipment or to provide care for underserved communities. “We think she is a wonderful role model for our profession.”
“From my perspective,” Vivien added, “Julie is a force of nature for good. She is a bright light in a dark place for countless animals and an equal number of people.”
Dr. Ryan was born at UCLA and raised in Orange County. Her father was a professor at Irvine Valley Community College and her mother was a nurse and later a school principal. She grew up in San Juan Capistrano and earned her undergraduate degree at Cal Poly San Luis Obispo. She attended veterinary school at the University of Wisconsin and did an internship at Virginia Tech.
After receiving her DVM degree, she worked in small animal and equine practices in Southern California, then moved to the Orange County Animal Shelter. She left there for a stint at Mars Petcare, then returned as shelter director.
She met her husband, Dr. Gary Johnson, at an SCVMA chapter meeting. He founded Dana Niguel Veterinary Hospital in Dana Point in 1982 and is now retired.
The Ryan-Johnson household includes three dogs, a horse and a male cat named Madam George that Dr. Ryan brought back to Southern California from her trip to Ukraine.
Canine Obesity: It’s a Big Problem
Has your vet ever said anything about your dog’s weight?
Published:
A professional organization called the Association for Pet Obesity’s Prevention (APOP) recently released a report stating that most of the dogs in the U.S. are overweight, their owners don’t know it, and their veterinarians don’t feel comfortable talking to their clients about it. This feels like crazyland to me!
I think I have to agree with the premise that most people really don’t recognize their dogs’ weight problem. When I attempt to have conversations with the owners of fat larger breed dogs, nine times out of 10, the owner will say, “Well, his mother and father both weighed over 100 pounds, these are just a large breed!” Or, “He’s in the weight range for the breed standard!” Ignoring the fact that the dog has no waist whatsoever and is literally covered with fat rolls.
Small dog owners often just think their dogs are cute. And as long as they can pick them up, they don’t think the weight is a problem.
When lick their own butts, it helps keep the anal glands in working order. Big dogs have fewer problems with their glands than small dogs partly because they have bigger, stronger tongues, which help massage and empty the glands when they lick their butts. When dogs like Dinah get too fat to reach their bottoms with their tongues, the glands can become impacted and infected unless the owner is aware of this and makes sure to either empty the glands or take the dog to a groomer or vet occasional to have the glands checked and emptied.
Anyway, to me, the most shocking part of the report is the allegation that 84% of the veterinarians who responded to the survey said they don’t want to upset their clients by talking about their dogs’ weight. But health and weight are so linked in dogs! I think that if a vet fails to discuss a dog’s overweight it’s a total dereliction of their veterinary duty! The problems associated with or directly caused by obesity in dogs are legion!
And yet, I get it. A vet only gets so much time with a client, and it probably often feels like there isn’t enough time to talk about the dog’s more pressing health issues and the overweight condition—even if the obesity may have contributed to the problem. Even at well-pet visits, people often spend more time discussing flea and heartworm preventives, vaccines, and the like.
My friend Tim Steele, a gifted dog trainer (who broke my heart by moving from my area to Florida a couple years ago), once told me that he never talks directly to dog owners about their dogs’ weight problems; he addresses his concerns to the dog—in front of the owner, obviously! He’ll say, “Oh my goodness, who is measuring your food? Or are you sneaking into the refrigerator at night?! I think you need to get on a little diet!” Often, he reports, the owner will join the “conversation” at that point, saying something like, “Do you really think he needs to be on a diet?” instead of feeling directly confronted. I think that’s a genius approach—and perhaps one I can recommend to veterinarians!
My appreciation to reporter Tim Wall of Petfood Industry for being the first to cover the APOP’s 2023 survey.